A recent study we saw on the Glaucoma Research Foundation’s website has uncovered a connection between psychological stress and increased intraocular pressure (IOP) in patients with primary open-angle glaucoma (POAG).
This new research sheds light on how the effects of stress might worsen the condition of those suffering from glaucoma, a disease that can lead to irreversible vision loss if not properly managed.
Glaucoma patients have often suspected that severe emotional stress causes visual field loss, so this study fascinated us.

Understanding glaucoma and intraocular pressure
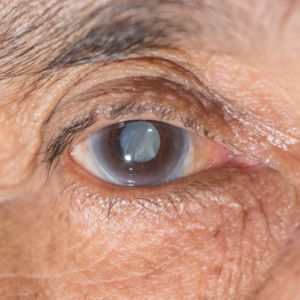
Glaucoma is a progressive eye disease in which damage to the optic nerve leads to optic nerve damage that can cause vision impairment and blindness. The most common form, primary open-angle glaucoma (POAG), is often managed by controlling intraocular pressure (IOP), which is the fluid pressure inside the eye.
Elevated IOP is a significant risk factor for the worsening of glaucoma and considerably lowers one’s quality of life.
Traditionally, treatments for glaucoma focus on lowering IOP through medications, surgery, or laser therapy. However, previous studies have shown that the side effects of stress affect the eyes, even in individuals without glaucoma, causing a temporary rise in IOP. This connection led researchers to investigate the impact of psychological stressors on IOP in glaucoma patients specifically.
The study: Investigating stress and IOP in glaucoma patients
A team of researchers designed a randomized-controlled trial (RCT) to explore the relationship between psychological stress and IOP in people with POAG. They wanted to see if stress could significantly impact eye pressure and, consequently, on glaucoma progression.
About the study participants
The trial involved 39 participants, all diagnosed with primary open-angle glaucoma (POAG). These participants were divided into two groups after a comprehensive eye exam:
- Stress Group: 18 participants who were exposed to a stress level increasing procedure.
- Control Group: 21 participants who did not undergo the stress test.
The stress test and measurements
Participants in the stress group were subjected to a psychological test known as the Trier Social Stress Test (TSST), designed to induce stress in a controlled environment. This test involves public speaking and mental arithmetic, commonly used to measure stress responses.
The study measured several baseline physiological responses using a tonometer in both the stress group and the control group, including:
- Intraocular pressure fluctuations (IOP)
- Salivary cortisol (a stress hormone)
- Salivary amylase (an enzyme associated with stress)
- Mean arterial pressure (especially high blood pressure)
- Heart rate
These measurements were taken at three different follow-up times:
- Before the stress test
- Immediately after the test
- 40 minutes after the test
Additionally, the State-Trait Anxiety Inventory (STAI) was used to assess levels of anxiety at these same intervals.
Stress causes a spike in IOP
Participants in the stress group experienced a notable rise in IOP following the stress test. The IOP increased by 3.8 mmHg in the right eye and 4.1 mmHg in the left eye. This spike in eye pressure was statistically significant (P<0.001 for both eyes).
Along with increased IOP, participants also showed elevated levels of stress markers, including:
- A 5.9 nmol/L increase in salivary cortisol (P=0.004).
- A 323,388 UL rise in salivary amylase (P=0.004).
- Elevated blood pressure and heart rate: The stress test significantly increased mean arterial pressure (up by 10.1 mmHg) and heart rate (up by 12.9 beats per minute) in the stress group.
These findings support the idea that psychological stress can temporarily raise IOP, which may pose a risk for glaucoma patients.
Limitations of the study
Despite the groundbreaking results, the study had several limitations:
- Chronic stress wasn’t evaluated: The research only measured the effects of stress. Long-term stress and anxiety disorders were not analyzed, leaving questions about how chronic stress might affect glaucoma progression over time.
- Sample size: The study’s small sample size, with only 39 participants, limited the researchers’ ability to explore how factors like age or cortisol correlate with stress-induced IOP increases.
- Disease progression: While the study found that stress can cause a temporary spike in IOP, it didn’t measure whether these spikes were severe enough to contribute to glaucoma progression.
Yes, stress could worsen glaucoma
The study authors commented on the potential implications of their findings. They believe that repeated exposure to stress in patients with glaucoma could negatively impact IOP control, potentially increasing the risk of disease progression.
While more research is needed to understand the mechanisms involved and develop targeted interventions, their work highlights the importance of managing stress in glaucoma patients.
This study emphasizes the need for glaucoma patients to focus on lowering IOP through conventional treatments and consider psychological well-being as part of their disease management plan.
Schedule your consultation today with the internationally recognized doctors at AGEI
Or call
866-945-2745
Incorporating relaxation methods for better IOP management
Given the study’s findings, incorporating relaxation techniques into the daily routines of glaucoma patients might help manage intraocular pressure (IOP) over the long term.
Methods such as mindfulness meditation, deep breathing exercises, progressive muscle relaxation, and yoga have been shown to help with stress reduction. Regular physical activities like walking or tai chi, which also promote mental well-being, can further reduce stress.
Cognitive-behavioral therapy (CBT) may offer additional benefits by helping patients develop coping strategies for stress management. By integrating these relaxation methods, glaucoma patients could lessen the frequency and severity of stress-induced IOP spikes, contributing to more consistent control over their condition and improving overall quality of life.
Assil Gaur Eye Institute, the nationally recognized experts in glaucoma treatment
Assil Gaur Eye Institute adheres to the country’s highest ophthalmology and patient care standards. They have assembled a team of top ophthalmologists from around the country who continue AGEI’s tradition of offering patients the highest quality of specialist eye care for their eye health.
Our Director of Glaucoma Services, Dr. Avneet K. Sodhi Gaur, is a Board-Certified, fellowship-trained Cataract and Glaucoma Specialist and an American Academy of Ophthalmology member.
She has extensive experience in conventional glaucoma laser treatments and surgical procedures, such as trabeculectomy and glaucoma drainage implants. Dr. Gaur also performs state-of-the-art minimally invasive glaucoma procedures, including iStent, iStent inject, Hydrus, endocyclophotocoagulation (ECP), OMNI 360, and Xen gel stent.
Sources
Differential impact of endurance, strength, or combined training on quality of life and plasma serotonin in healthy older women. https://link.springer.com/doi/10.1007/s40520-019-01120-xnce imaging
Surprising Links Between Stress and the Eyes. https://www.aao.org/eye-health/tips-prevention/anxiety-stress-dry-eye-glaucoma-iop
What Is Ocular Hypertension? https://www.aao.org/eye-health/diseases/what-is-ocular-hypertension













