- Previous
- Eye Care
Dr. Svetlana Pilyugina discusses retinal detachment and its treatment
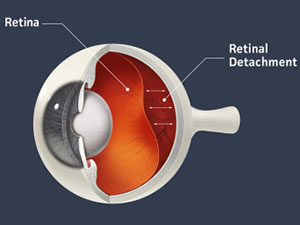
The retina is a thin layer of light-sensitive tissue that lines the back of the eye cavity like wallpaper. When a crack develops in this thin tissue, it's called a tear.
In most cases, retinal tears occur spontaneously, but trauma or prior eye surgery can also cause retinal tears.
If fluid passes under the tear and separates the retina from the wall of the eye, it can lead to a retinal detachment. Retinal detachment is an extremely serious problem that almost always leads to permanent vision loss if not treated quickly.
- Signs and symptoms of retinal detachment or retinal tear?
- How is a retinal tear or detachment diagnosed?
- What are the retinal tear and detachment risk factors?
- What are the treatment options for retinal tears?
- What are the treatment options for a detached retina?
- Choose Assil Gaur Eye Institute for retinal treatment
- Retinal detachment FAQs
- What are the risks of Retinal detachment surgery?
- How long must a patient lay face-down after Pneumatic Retinopexy surgery?
- Why can’t laser surgery be used to treat a detached retina?
- Are there different types of retinal detachment?
Signs and symptoms of retinal detachment or retinal tear?
Retinal tears and detachments are painless but typically present with visual symptoms such as:
- Sudden onset of new floaters- these can look like small moving specks or clouds, small dots, or cobwebs
- Flashes of light (photopsia) that persist throughout the day
- If bleeding occurs with the retina tear, your vision may become murky.
- Poor peripheral vision
If the tear has led to a retinal detachment, there may be a fixed shadow or sensation of a curtain closing in your field of vision.
How is a retinal tear or detachment diagnosed?
Diagnosing a retinal tear requires an eye exam of the retina through a dilated pupil. Our doctor may use an instrument with a bright light and special lenses to examine the back of your eye, including the retina.
If you have symptoms of a retinal tear, it is vital to see our ophthalmologists or retinal specialist immediately.
What are the retinal tear and detachment risk factors?
While most tears occur spontaneously due to movement and pulling of the gel inside the eye, some eye conditions can predispose you to a retinal tear:
- A high degree of nearsightedness (myopia) -- because myopic retinas tend to be very thin
- Lattice degeneration – areas of retinal thinning along its outer edges
- Family history of retinal detachment
- Prior eye surgery, such as cataract surgery
- Prior severe eye injury
Additionally, prior retinal detachment in one eye gives you a 10% chance of developing a detachment in your other eye.
What are the treatment options for retinal tears?
Conservative treatment for retinal tears
Depending on their size and location, some retinal tears may be considered “low risk” with little chance of progressing to retinal detachment so no treatment may be required.
Occasionally, the eye spontaneously forms a stabilizing scar around the tear. Nonetheless, once a tear has been identified, it needs to be followed by a retina specialist to ensure it does not get worse.
Retinal tear surgery
When a retinal tear is identified, it will need to be surgically repaired. The treatment aims to seal the edges of the retinal tear and prevent the liquid inside the eye from seeping under the retina through the tear, as this can lead to retinal detachment. Retinal tear surgeries include:
-
- Laser treatment (photocoagulation) causes scarring to the underlying tissue, which seals the retinal tear. This prevents fluid from getting under the retina.
- Cryotherapy (cryopexy) offers a similar result by freezing the area to seal the tear, preventing further damage.
Of all the eye treatments, this has one of the easiest recoveries! There are virtually no restrictions following these retinal treatments. You can resume your normal activities and work schedule immediately.
Schedule your consultation with the internationally recognized retina specialists at Assil Gaur Eye Institute
What are the treatment options for a detached retina?
Almost all patients with retinal detachment will need surgery to place the retina back in its proper position. The good news is that 90% of retinal detachment surgeries are successful with a single operation.
While the laser procedure can treat a retinal tear, it cannot be used to repair an already detached retina that is no longer in contact with the eyewall.
Three outpatient surgical options are available for repairing detached retinas, and the type of surgery is determined by a retinal specialist based on the specific condition of each detachment.
Scleral Buckling
In this procedure, our surgeon sews a silicone band (buckle) to the outer white part of your eye (called the sclera). This causes the eyewall to indent, counteracting the force pulling the retina out of place. The fluid under the detached retina is drained, which allows the retina to settle back into its normal position against the back wall of the eye. Once the retina is flattened against the eyewall, a laser welds the retinal tears' edges, sealing the leak.
Pneumatic Retinopexy
In this surgery, a doctor injects a small gas bubble into the vitreous gel, the gel-like substance that fills the inside of your eye. The bubble floats up against the detached retina, gently pushing it back into place. Our surgeon then uses a laser or a freezing treatment to seal the tears or breaks in the retina, which helps the retina to reattach to the back wall of the eye.
Following surgery, the patient is placed face down and must maintain this position so the bubble can float to press the detached tissue against the eyewall.
Vitrectomy
In this procedure, three tiny incisions are made in the white part of the eye to remove the vitreous (jelly-like fluid) that fills the eye.
The fluid collected under the retina is drained, and a special gas (or, in some cases, silicone oil) is placed inside the eye to help push the detached retina against the eyewall while it heals. Laser photocoagulation is also used to seal the retinal breaks.
The body gradually absorbs the gas over several weeks, and the inside of the eye eventually re-fills with vitreous fluid, which the eye continually produces.
Learn more about vitrectomies here.
Choose Assil Gaur Eye Institute for retinal treatment
AGEI has one of the most advanced retinal lasers, known as PASCAL. It provides not only superior patient comfort but also the efficacy of treatment by delivering multiple spots per second in a customized pattern, which reduces the total treatment time.
The AGEI staff includes a highly skilled retina specialist, Dr. Svetlana Pilyugina, or “Dr. P,” as she is known to her patients. Dr. Pilyugina is an ophthalmologist with fellowship training and board certification in diseases and surgery of the vitreous and retina.
Dr. Pilyugina has extensive experience treating retinal diseases, including age-related macular degeneration (AMD), diabetic eye disease and diabetic retinopathy, retinal tears and detachment, flashes, floaters, macular holes, retinal vein occlusion, and complex retinal conditions.
Besides her eye care experience, Dr. Pilyugina is known for her dedication to her patients and focus on personal service. That is why she limits the number of patients she sees daily in the clinic to allow her to dedicate sufficient time for evaluation and consultation with each patient to meet her high standard of care.
We are conveniently located for patients throughout Southern California and the Los Angeles area in or near Beverly Hills, Santa Monica, West Los Angeles, West Hollywood, Culver City, Hollywood, Venice, Marina del Rey, Malibu, Manhattan Beach, and Downtown Los Angeles.
Retinal detachment FAQs
What are the risks of Retinal detachment surgery?
Complications may occur, but they are infrequent and less than one in 2000 cases. Risks and complications include:
- Bleeding
- Infection
- Not fully recovering your vision
- Retinal detachment recurrence, which can require more surgery
- An increase in eye pressure (glaucoma)
- Damage to nearby eye structures
- Increased risk of cataracts due to post-op changes in the eyes' lens
How long must a patient lay face-down after Pneumatic Retinopexy surgery?
The face-down positioning can range from 1 to 5 days, and avoid flying and higher altitudes for one to three months following surgery (depending on the type of gas used).
Why can’t laser surgery be used to treat a detached retina?
This is because, with a retinal tear, the eyewall underneath the retina absorbs the energy from the laser to create a scar that fuses the edges of the tear to the eyewall.
Because a detached retina has no contact with the eyewall, no surface can receive the laser energy. This is why when the retina has already detached. Other surgical methods are required to repair it.
Are there different types of retinal detachment?
Yes, there are three main types of retinal detachment:
- Rhegmatogenous retinal detachment is the most common type, which happens when a tear or hole in the retina allows fluid to get under it and cause it to detach from your eyeball.
- Tractional retinal detachment occurs when scar tissue on the retina's surface contracts and causes the retina to pull away from the back of the eye. This type often affects people with uncontrolled diabetes.
- Exudative retinal detachment happens when inflammation, injury, or vascular abnormalities cause fluid to accumulate underneath the retina without tears or holes. Each type of detachment has different causes and may require different treatment approaches or surgical procedures.
Sources
Detached retina. American Academy of Ophthalmology. https://www.aao.org/eye-health/diseases/detached-torn-retina.
Freund KB, et al. Peripheral retinal degenerations and rhegmatogenous retinal detachment. In: The Retinal Atlas. 2nd ed. Philadelphia, Pa.: Elsevier; 2017. https://www.clinicalkey.com.
- Previous
- Eye Care
-
Retina Specialist
As a member of an elite group of only 3000 retina-vitreous specialists in the United States, Stanford trained Dr. Pilyugina brings to AGEI a unique skill set in the treatment and surgery of retinal disease. Her academic credentials include numerous research papers, conference presentations, medical publications, and clinical trials.














