Restoring sight to the blind has always been considered a top-tier miracle. Both St. Lucy, a patron saint of the blind, and St. Francis of Assisi are reputed to have performed several such sight-restoring miracles.
More recently, St. Charbel, a Lebanese Maronite monk who died in 1898, is credited with restoring the eyesight of a 30-year-old mother of three who, in 2017, prayed over the saint’s relics in a Phoenix church.
Without passing judgment on the accuracy of such miracle accounts, it seems fair to note that they appear to occur rarely, and they seem to benefit only a few.
Now modern medical science appears to be offering a secular miracle – the potential restoration of sight to a multitude of blind people.
An article in the May 24th edition of Nature Medicine reports the first case of eyesight recovery using a new technique of experimental biology known as optogenetics.
Who founded optogenetics?
In 1979, Francis Crick, the co-discoverer of DNA’s double helix, mused that “although it seems far-fetched, it is conceivable that molecular biologists could engineer a particular cell type to be sensitive to light.”
Fast forward to 2005, when Karl Deisseroth, a neuroscientist in the Departments of Bioengineering and of Psychiatry and Behavioral Sciences and the Howard Hughes Medical Institute, Stanford University, together with Ed Boyden and Lief Fenno, also Stanford-based neuroscience researchers, published a paper on what came to be known as optogenetics.
Deisseroth had learned about the work of Peter Hegemann, Georg Nagel, and Ernst Bamberg, who had identified the light-sensitive proteins, known as opsins, which are found in luminescent green algae, the same sort of green algae that grows in ponds. He discovered how to use a virus to import those microbial opsins (called channelrhodopsin-2 or chr2) into contact with human brain cells (neurons).
What is optogenetics?
The Stanford team surmised that making those neurons sensitive to light could lead to new knowledge regarding how the human brain really functions. His team devised a method of attaching pieces of DNA to the opsin gene as a sort of password, a way of making sure that only the targeted neural circuits would be affected.
A light-sensitive neuron is, of course, of little use without a method of light delivery to trigger it. So, once the targeted cells were made light-sensitive, a method of optogenetic stimulation had to be invented. Ultimately, fiber optic wires attached to electrodes were used to deliver flashes of light to regions deep inside the brain.
How does optogenetics work?
Optogenetic control of neuronal activity was initially envisioned as a way to probe the inner secrets of deep brain function. Brain stimulation, by implantation of a light source deep in the various brain regions of a laboratory animal, told researchers how to influence neural activity by switching a specific cell on or off.
This modulation tactic, activation or inhibition of one particular neuron, has led to the discovery of the brain circuitry underlying many kinds of behavior. Deisseroth envisioned victories against diseases of the nervous system, such as Parkinson’s disease.
Deisseroth’s work has earned several prestigious international prizes, making him optogenetic’s prime promoter.
After Deisseroth established the basic foundations of optogenetics, other teams of medical scientists took the baton in the relay race against neurological deficits. Their development of optogenetic approaches has dramatically furthered both the current reality and the future potential of optogenetics.
Optogenetics and blindness
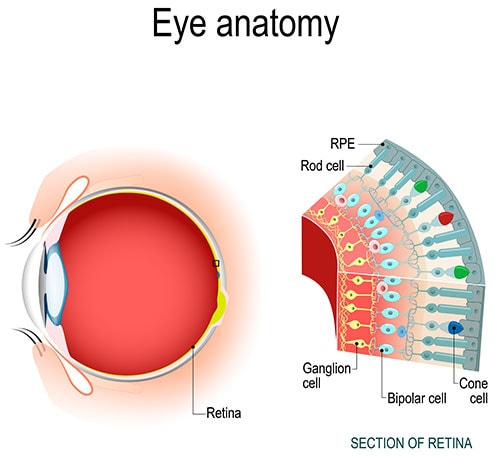
When a photon (light) enters the eye, it is captured by photoreceptor cells in the retina. The photoreceptor cells then send an electrical signal to adjacent cells, known as ganglion cells. Ganglion cells can identify important features of vision, such as motion. The combined signals are then sent to the optic nerve, which delivers the flow of visual information to the cortex.
Two of the leading causes of blindness – age-related macular degeneration (AMD) and retinitis pigmentosa (RP) – are both caused by the death of photoreceptors. However, even after AMD or RP has caused the photoreceptors to die, the remainder of the retina remains intact. At least potentially, the retina could still be functional.
So, if the retinal ganglion cells could be made to produce a light-sensitive protein, the flow of sight-related information to the brain might be renewed.
How does optogenetics work for a blind person?
An international team of researchers (based in Paris, France, Pittsburgh, USA, and Basel, Switzerland) accepted the challenge of using optogenetic tools to restore the sight of their blind patient. The patient was a 58-year-old Parisian man who completely lost his vision to retinitis pigmentosa 40 years ago.
Dr. José-Alain Sahel, an ophthalmologist who splits his time between the University of Pittsburgh and the Sorbonne in Paris, led a team that devoted 13 years of multidisciplinary effort to restore a blind person’s sight. The goal was to use optogenetic techniques to turn ganglion cells into new photoreceptor cells.
Sahel and his colleagues recognized that the optogenetic proteins currently in use at the time were not sensitive enough. They couldn’t produce a visible image from the sort of ordinary light that normally enters the eye.
But the team could not beam amplified light into the patient’s eye because the intensity would destroy the delicate retinal tissue. So, they chose an optogenetic protein that’s sensitive only to amber light. The longer wavelength of red light is easier on the eye than the more energetic blue light typically used for optogenetic research.
The patient was also fitted with a pair of custom-made goggles. The specially engineered goggles detect changes in ambient light intensity and project corresponding light pulses onto the patient’s retina.
The light pulses were designed to activate the patient’s retinal ganglion cells, which have been turned into receptor cells by an injection of a viral vector containing that amber light-sensitive protein, known as ChrimsonR.
The patient’s training with the goggles began nearly five months after the injection. The delay gave the ChrimsonR protein time to work its transformative magic on his ganglion cells.
Seven months later, the blind patient began reporting signs of visual improvement
With the aid of the goggles, his optogenetically enhanced vision allowed him to consistently locate, touch, and count objects placed on a white table in front of him.
What is the goal of optogenetics?
The goal is a future full of secular miracles. It’s going to be a long time, a time filled with dedicated and dogged medical, scientific, and bioengineering endeavors, before the Parisian patient, or any other currently blind person, regains enough optical control to read a book, drive a car, or visually identify a loved one.
But such endeavors are occurring so frequently now that they are becoming commonplace. Even though it may take a lot of time, the scientific miracles will continue to proliferate. The deaf shall hear, the lame shall walk, and the blind shall see. The age of miracles has just begun.
Why choose Assil Gaur Eye Institute for your eye care?
At AGEI, you will experience a state-of-the-art health care facility that brings together revolutionary technologies with experienced vision care professionals. Our goal is to help you achieve your personal best vision.
Please call 866-945-2745 or visit us here to make an appointment online. If you are experiencing any concerning symptoms, contact us immediately to determine the best time to schedule an exam.
At Assil Gaur Eye Institute we take our patients’ safety seriously. Our facility’s Covid-19 patient safety procedures exceed all CDC recommendations during this coronavirus pandemic. Masks are required in our institutes at all times.
We are conveniently located for patients throughout Southern California and the Los Angeles area at locations in or near Beverly Hills, Santa Monica, West Los Angeles, West Hollywood, Culver City, Hollywood, Venice, Marina del Rey, Malibu, Manhattan Beach, and Downtown Los Angeles.
- Why Does Pregnancy Cause Blurry Vision? Should I Be Worried? - 04/18/2023
- Eye Disease from Diabetes: A Leading Cause of Blindness - 01/09/2023
- Could these eye drops replace reading glasses? - 04/04/2022