Poets will no doubt continue to describe a person’s eyes as ocular windows to the soul. But physicians of the near future may view those same eyes as diagnostic tools, which, if read properly, can accurately foretell the imminence of strokes or dementia.
On March 11, 2021 the Healthday Reporter described a new study, conducted at the Mayo Clinic facility in Jacksonville, Florida. This study links the presence of eye disease to an increased risk of stroke, dementia, and premature death.
What is the retina?
The first step in the seeing process is the conversion of observed light into signals the brain will interpret as vision. This first step takes place in the retina, which lines the inner surface of the back of the eyeball. The retina is composed of several layers, including one containing an array of extraordinary cells called photoreceptors.
The cornea and lens, located at the front of the eyeball, focus image-laden light onto the photoreceptor cells in the retina. Those cells convert the focused light into chemical and nervous signals. The optic nerve transports these signals to visual interpretive centers, located at the back of the brain.
What is retinopathy?
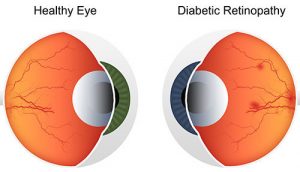
The Greek suffix “-pathy” means “suffering” or “disease”. So retinopathy means disease of the retina. There is a multitude of retina pathologies, but the ones we are most interested in are diabetic retinopathy and hypertensive retinopathy.
One of the devastating consequences of diabetes is harm to the blood vessels that nourish the retina. Retinal damage caused by diabetes often results in significant vision loss.
Hypertensive retinopathy is a result of cholesterol buildup that leads to atherosclerosis (hardening of the arteries). Those hardened arteries lead to chronic high blood pressure. Like diabetes, this condition can impair vision by damaging the retinal microvasculature (the network of tiny veins and arteries that supports the retina).
How is retinopathy detected?
An ophthalmoscope is a medical diagnostic instrument that enables close examination of the interior structure of an eyeball, including the retina, the optic nerve, and the attendant blood vessels.
This handheld device consists of strong light and a small mirror or prism that directs it into the eye. The light reflects off the retina and back through a small hole in the ophthalmoscope.
The examiner sees a magnified, vivid, crystal clear, and full-color image of the structures at the back of the eye. With this tool, the examiner can see the retina and the microvascular network laced throughout it.
How is retinopathy related to stroke and dementia?
It’s long been known that the veins and arteries of the retina are physiologically similar to the corresponding vasculature of the brain. The same sort of blood vessel harm that leads to vision impairment can also constitute a risk factor for a brain hemorrhage (stroke) or damage to the brain centers that handle mental processing (memory problems leading to dementia).
Cardiovascular disease has similar characteristics no matter where it occurs. So, it follows that the existence of cardiovascular risk factors in the retina could be an indication of a higher risk of the type of cardiovascular damage that leads to stroke or dementia.
In fact, a 2008 review of the literature current at that time concluded that patients with hypertensive retinopathy were more likely to experience the corresponding pathology in their brain vasculature. In other words, a patient’s hypertension may simultaneously affect both their eye and their brain.
A peer-reviewed study conducted in 2013 examined the question of whether the existence of hypertensive retinopathy indicates a higher risk of future stroke.
That study concluded that patients with hypertensive retinopathy are at an increased risk of stroke. This was true even for those with apparent good control of their chronic hypertension. These findings suggest that a retinal examination may be valuable for assessing stroke risk in patients with hypertension.
A new study dives deeper into the connection between severe retinopathy and stroke
The new Mayo Clinic study increases both the scope of the question addressed (it included both hypertensive retinopathy and diabetic retinopathy) and the specificity of the findings.
The Mayo Clinic researchers studied data compiled by the U. S. National Health Surveys between 2005 and 2008, with linked mortality data through 2015.
The key findings of the study, presented at the American Stroke Association’s 2021 International Stroke Conference, held March 17-19, 2021, included both:
- The more severe the retina damage, the more likely the participants were to die of stroke within the next decade.
- Retinal scans may help identify those at increased risk of future stroke or dementia, so preventative care can be supplied.
Michelle P. Lin, the Mayo Clinic study’s lead author, said, “The retina is a window to the brain. A retinal photo that shows a magnified look at the back of the eye, including the retina and optic nerve, is cheaper and faster to perform than an MRI, so we’re wondering if it might be a good screening tool to see who could benefit from a referral to a neurologist for a brain MRI.”
In addition to retinal photos taken by ophthalmologists, Lin also suggested that retinal photos could eventually be taken by the patient themself, via an adaption to a smartphone camera, and then forwarded to the doctor.
Why choose Assil Gaur Eye Institute for your eye care?
At AGEI, you will experience state-of-the-art health care facilities that bring revolutionary technologies together with experienced vision care professionals. Our goal is to help you achieve your best possible vision.
Please call 866-945-2745 or visit us here to make an appointment online. If you are experiencing any concerning symptoms, contact us immediately to determine the best time to schedule an exam.
At Assil Gaur Eye Institute we take our patients’ safety seriously. Our facility’s Covid-19 patient safety procedures exceed all of the CDC’s coronavirus pandemic recommendations. Masks are required in our institutes at all times.
We are conveniently located for patients throughout Southern California and the Los Angeles area at locations in or near Beverly Hills, Santa Monica, West Los Angeles, West Hollywood, Culver City, Hollywood, Venice, Marina del Rey, Malibu, Manhattan Beach, and Downtown Los Angeles.