The different systems of the human body are far more interconnected than many people realize. Obviously, eye diseases will negatively impact your vision, but more general medical conditions can also cause vision loss or eye diseases such as glaucoma and retinopathy.
For example, if you have high blood pressure, the force of the blood pushing against your artery walls is consistently too high. When that happens, the heart must work extra hard to pump blood increasing your risk for vascular (blood vessel) damage, kidney problems, and even vision problems.

How does blood pressure impact eye health?
The American Heart Association warns that high blood pressure can cause multiple eye conditions: blood vessel damage in the retina (hypertensive retinopathy), optic nerve damage (optic neuropathy), and fluid buildup under the retina (choroidopathy).
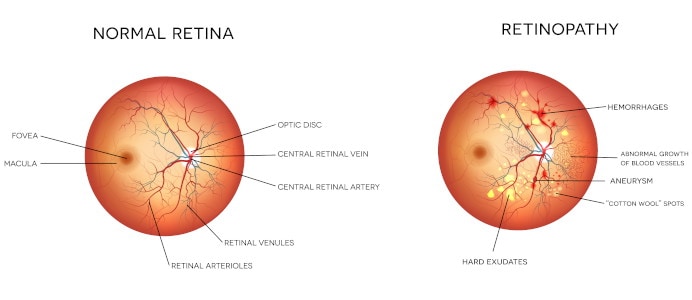
The retina is the layer of tissue in the back of the eye responsible for collecting the light that enters the eye and sends signals to the brain to be converted into images. When this part of the eye is damaged, you may experience floaters, blurred vision, or vision loss.
Damage to the retina due to high blood pressure is called hypertensive retinopathy. The term refers to changes in the tiny blood vessels in the retina that may include leaking, fluid buildup, or decreased blood supply.
High blood pressure may lead to other serious health problems, including heart attack, stroke, kidney disease, and vision loss.
Can you treat hypertensive retinopathy?
Treating hypertensive retinopathy usually means controlling high blood pressure through lifestyle changes, medication, and careful monitoring. By getting blood pressure under control early, you can prevent further damage and potential heart failure. In addition, with proper blood pressure management, existing damage may slowly heal.
Symptoms of hypertensive retinopathy
Unfortunately, retinopathy doesn’t display overt symptoms. The first symptoms you may notice are headaches and loss of vision. Luckily, the ophthalmologists at the Assil Gaur Eye Institute are trained to detect retinal damage using sophisticated instruments during eye exams.
Eye doctors looking deep into the retina can detect the following:
- A swollen optic nerve
- Red eyes
- Narrowing of the blood vessels
- Damaged blood vessels
- Fluid buildup (choroidopathy) in the center part of the retina
- Thick, twisted blood vessels
- Cotton wool spots on the retina
When retinopathy becomes more advanced, you may notice more changes:
- Vision loss
- Dim vision
- Double vision
- Fluctuating vision
- Eye floaters
- Blind spots
- White pupil
- Abnormal eye movements
How the Assil Gaur Eye Institute diagnoses retinopathy
During your yearly examination, your ophthalmologist may run several tests to diagnose your level of retinal damage. These tests include a fluorescein angioplasty and ophthalmoscopy.

What is fluorescein angiography?
This test detects blood flow problems, including leaks and blockages in retinal blood vessels. The doctor may dilate your pupils to get a better view.
After injecting a dye into a vein in your arm, they use a camera-like instrument to capture images showing blood flow in the retinal vessels.
What is ophthalmoscopy?
Ophthalmoscopy or fundoscopic exam lets the ophthalmologist see the back part of your eye (fundus). Your health care provider will use an ophthalmoscope to look for narrowing of the blood vessels and signs that fluid has leaked from blood vessels. This examination reveals problems with blood vessels that nourish the retina.
What you can do to prevent retinopathy
People may be able to prevent retinopathy caused by hypertension or diabetes by following a healthy lifestyle and keeping their blood pressure and blood sugar under control.
Consider the following protective measures:
- Take part in regular physical exercise.
- Eat healthy meals.
- Control your cholesterol. This reduces the risk of arteriosclerosis and narrowing blood vessels supplying the retina.
- Stop smoking.
- Take any blood pressure medications prescribed by your healthcare provider.
- Get regular eye exams.
- Monitor your blood pressure at home and at the doctor’s office. (If the top number is over 180 or the bottom number is around 100, it may be a medical emergency.)
- If diabetic, get a hemoglobin A1C test every three months to understand your ongoing blood sugar level.
- The Centers for Disease Control (CDC) recommends at least seven hours of sleep each night.
Why trust the Assil Gaur Eye Institute with your eye health?
The Assil Gaur Eye Institute represents the country’s highest eye care and patient care standards. This commitment dates back to 1949 when the Institute was chartered by the father of modern cataract surgery, Dr. Robert M. Sinskey.
Dr. Kerry Assil began his career as an academic ophthalmologist working on pioneering techniques and inventions in refractive surgery. From there, Dr. Assil became a renowned surgeon and leader in the Cataract and LASIK surgery field.
AGEI is nationally recognized for its compassionate, patient-centric care, commitment to pioneering advances in ophthalmology, and dedication to supporting patients’ eye problems and well-being.
Please call (866) 945-2745 or make an appointment online.
We are conveniently located for patients throughout Southern California and the Los Angeles area at locations in or near Beverly Hills, Santa Monica, West Los Angeles, West Hollywood, Culver City, Hollywood, Venice, Marina del Rey, Malibu, Manhattan Beach, and Downtown Los Angeles.
- Vision Suddenly Blurry? You May Be Having a Medical Emergency - 07/03/2024
- Does High Blood Pressure Affect Your Vision? - 09/19/2023
- Noticing Peripheral Vision Loss? What You Need to Know - 05/01/2023