- Home
- Resource Library
- Cornea Conditions & Treatments
- Cornea Conditions Explained
Cornea Conditions Explained

What is a Cornea?
The cornea is your eye’s clear protective outer layer (like a windshield) that serves two important functions: a barrier protecting your eye against dirt, germs, and UV rays.
The cornea’s surface shape determines how light rays are bent (or refracted) as they enter your eye. If the shape is too steep, too flat, or not completely round, it can cause problems such as nearsightedness, farsightedness, or astigmatism.
Physical injuries and certain eye conditions can result in scarring, thinning, or permanent corneal damage leading to vision loss. In fact, corneal conditions are the fourth leading cause of blindness after glaucoma, cataracts, and macular degeneration.
Your cornea is surprisingly tough and capable of healing itself after most minor injuries that can cause small tears or abrasions (scrapes) to the corneal surface.
Mild corneal abrasions typically heal quickly because the outer corneal surface (known as the epithelium) is the fastest healing tissue layer in the human body. That said, you should seek out your eye care specialist if any symptoms mentioned below persist.
Common cornea conditions
The most common conditions affecting the cornea include:
Keratitis
Keratitis is caused by infection, injury, disease, or wearing contact lenses too long.
Symptoms of keratitis include severe eye pain, blurred vision, and mild to severe eye discharge. Your doctor may treat you with frequent doses of antibiotic or antifungal eye drops until the ulcer heals.
Keratitis, when severe, can result in corneal ulcers and scarring that can lead to serious vision problems and permanent vision loss.
Dry eye

Dry eye symptoms include a persistent sensation of some irritant in your eye, stinging, burning, excessive tearing following periods of dryness, pain, redness, the feeling that your eyelids are heavy, or episodes of blurred vision.
The risk of getting Dry Eye increases with age, being a post-menopausal woman, and looking at computer and phone screens.
The eye may become dry, red, and inflamed. The main symptoms are discomfort and sensitivity to light.
Learn more about dry eye
Corneal abrasion
While a number of conditions can cause light sensitivity, if you have significant eye pain with light sensitivity that won’t quit, it may well be that you have a corneal abrasion (a scratch) on the clear outer layer on the surface of the eye. This can be caused by dust, sand, dirt, wood, or metal shavings or even abusing your contact lenses.
Although most corneal abrasions typically heal in a day or two, if your symptoms persist or are particularly bad, you need to be seen right away. That’s because a corneal abrasion can progress to a corneal ulcer, or hole, in your cornea and that can lead to a serious eye infection and vision loss if left untreated.
Allergic reactions
Reactions to plants, animals, or chemicals in your environment frequently irritate the corneas. Allergy-related symptoms can include redness, itching, tearing, burning, stinging, and watery discharge.
These symptoms are usually managed with antihistamine decongestant eye drops.
Causes of common corneal injuries
- Foreign objects, such as sand, dust, or glass particles
- Something hitting the eye, such as a tree branch or metal shavings
- Radiation exposure from the sun, UV lamps, welding, or sun reflected on snow
- Complications from contact lens use
- Severe cases of dry eye can result in corneal ulcers
- Conditions that prevent your eye from fully closing (like Bell's palsy or strokes) can cause corneal drying and lead to ulcers
Symptoms of common cornea conditions
- Eye pain
- Tearing
- Blurred vision
- Eye redness
- A feeling of something being stuck in your eye
- Extreme sensitivity to light
Serious Cornea Conditions
There are over 20 corneal diseases, known as dystrophies, that cause structural damage leading to clouding, visual distortion, and sometimes blindness.
Corneal dystrophies are often inherited conditions, involve both eyes, usually progress slowly and affect otherwise healthy people. They include:
Keratoconus

Keratoconus is a condition when the clear, dome-shaped tissue that covers the eye (cornea) thins and bulges outward into a cone shape. Its cause is unknown.
Keratoconus can progress gradually or rapidly and can affect one eye, although it usually affects both.
Excessive eye rubbing is a major contributor to the development of Keratoconus. Initial treatment can include glasses, soft contacts, or even rigid gas permeable lenses. Severe cases might require a corneal transplant.
Keratoconus Treatments
Treatments include Collagen Cross-Linking, Intacs, and special contact lenses for Keratoconus patients.
Learn more about Keratoconus
Schedule your consultation with the internationally recognized cornea specialists at Assil Gaur Eye Institute
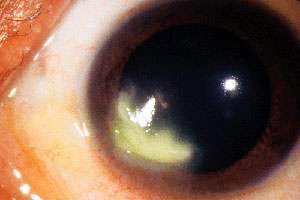
Pterygium (surfer's eye)

Surfer’s eye, otherwise known as pterygium, is a condition that occurs when a pink web-like growth forms on the white part of the eyeball.
Fortunately, It rarely grows over the pupil, so removal is not recommended unless it affects vision or is of cosmetic concern. While its cause is not known, long-term exposure to solar UV rays is suspected to play a role.
Typically, pterygium treatment is simply watching it over time to see if it grows over your visual axis (your iris and pupil). Surgical removal of a pterygium is performed if it obstructs your vision or if you want it removed for cosmetic reasons.
Pterygium treatment begins with monitoring the condition and using simple anti-allergy drops, lubricating eye drops, artificial tears, anti-inflammatory agents, and ointments. Due to the potential for recurrence of a more aggressive pterygium lesion, AGEI may then performs surgical removal of pterygia using an ultramodern approach that has succeeded in reducing the recurrence rate from 80% to less than 1%.
Learn more about Pterygium
Map Dot Fingerprint Dystrophy
Map Dot Fingerprint Dystrophy (aka Epithelial Basement Membrane Dystrophy) is due to abnormal folds in the cornea’s outer surface that resemble ridges on a map or a fingerprint.
At first, this condition is painless and causes no vision loss, but later symptoms can include eye pain, blurred morning vision that improves during the day, light sensitivity, excessive tearing, and a sensation of an irritating object in the eye.
Treatments can include lubricating eye drops and ointments. More severe cases may require surgery to address painful corneal erosions.
Fuch's Endothelial Dystrophy
Fuch’s Endothelial Dystrophy is a hereditary breakdown of the cornea’s inner lining responsible for fluid exchange between the cornea and inner eye. As it breaks down, the cornea swells and becomes cloudy, causing blurred vision. In the late stages, painful blisters form. It occurs more often in women, and symptoms may begin at age 30 to 40.
Severe cases may require a corneal transplant.
Lattice Dystrophy
Lattice Dystrophy is a condition in which protein fibers clump, forming a lattice-like pattern inside the cornea's middle layer. Over time, this obstructs the cornea and decreases vision.
Eventually, these deposits can erode the cornea’s outermost layer, causing severe pain. This condition is usually diagnosed during childhood and is managed with steroid eye drops, ointments, and patching of the eye to let it heal.
By the time a patient is middle-aged, their corneas might be so cloudy and scarred as to require a cornea transplant.
Ocular herpes & Herpes zoster (shingles)

Ocular Herpes is a common, recurrent viral infection affecting the eyes, usually due to the herpes simplex virus (HSV I). This is the same virus that causes cold sores but can also result from sexually transmitted herpes (HSV II).
Herpes Zoster symptoms include painful corneal blisters and fever. Some people can develop chronic pain and permanent scarring after a shingles outbreak.
Symptoms include painful sores and inflammation of the cornea that can progress to scarring or spread to surrounding areas.
Serious corneal disease symptoms include:
- Seeing halos around bright lights
- Experiencing glare when in sunlight
- Having blurry vision in the morning that clears up throughout the day
Why patients choose AGEI for their corneal care
Expertise in corneal disease management: Dr. Assil began his leadership role as a corneal transplant surgeon in one of the largest corneal transplant practices in the United States, serving as university faculty in St. Louis. He went on to be the medical director of the Mid-America Eye and Tissue Bank. Since opening his Los Angeles practice in 1995, Dr. Assil has performed over 1000 corneal transplants.
Latest Transplant Techniques: At AGEI, we utilize the latest surgical techniques designed to preserve the structural integrity of your eye, minimize the risk of rejection, speed up recovery, and improve your vision.
The AGEI Difference: As Medical Director of the Assil Eye Institute, Dr. Assil has taken corneal transplantation a step further by offering LASIK to those patients who wish to improve their vision after they have undergone corneal transplant surgery.













